The Centre has a mission to discover the fundamental molecular mechanisms that determine cell function in health and disease.

The Centre is home to around 170 scientists and support staff working collaboratively towards a common goal.

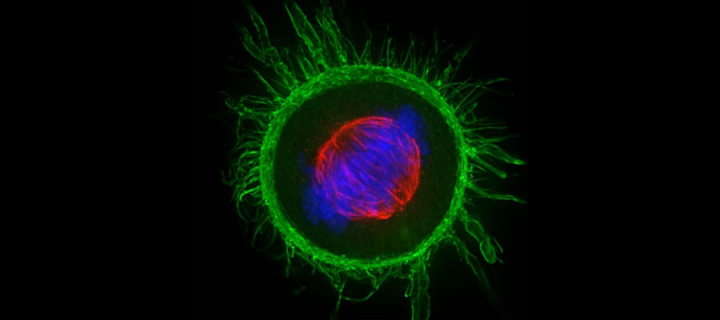
- Rewiring of the phosphoproteome executes two meiotic divisions in budding yeast
- C19ORF84 connects piRNA and DNA methylation machineries to defend the mammalian germ line
- A conserved CENP-E region mediates BubR1-independent recruitment to the outer corona at mitotic onset
- DNMT3B PWWP mutations cause hypermethylation of heterochromatin
- A time- and single-cell-resolved model of murine bone marrow hematopoiesis

Public engagement is integrated into our research vision and reaches into diverse communities.

Sustainability is an integral part of the Centre, and we are committed to conducting our research sustainably.